Transforming Alberta Primary Care
What if the solution is right in front of us?
The future we all hope for.
In any successful transformation, the most important thing is to have a clear picture of what the future looks like. Easy, right? Every Albertan has a medical home with access to a family doctor who is connected to a team, including nurses, pharmacists, mental health specialists and other allied professionals. More medical students and residents are choosing to practice comprehensive family medicine in Alberta. Family practice clinics in urban and rural communities across our province are thriving, providing care for, and advocating on behalf of, their patients. This is the future we all hope for.
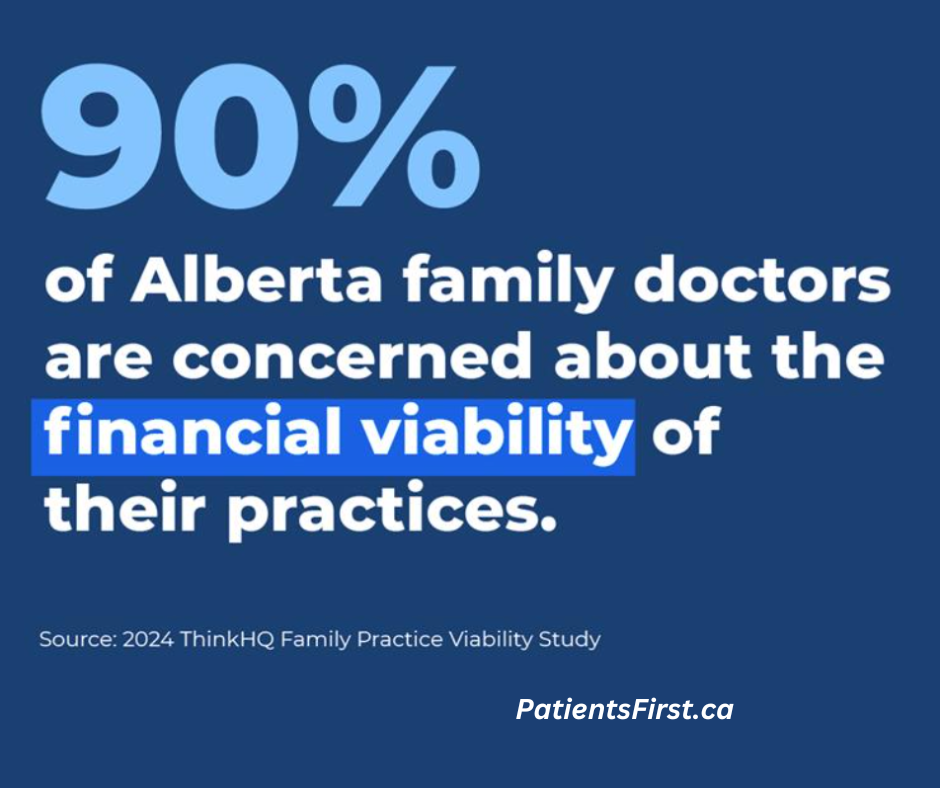
The challenge -- how do we get there? This is where things get hard. There is general agreement that while primary care is the bedrock of our healthcare system, in Alberta and beyond, family medicine is in peril. Today it is estimated that 650,000 Albertans are without a family doctor or primary care provider (source: Alberta Medical Association, 2023). We are experiencing family doctor shortages due to burnout, early retirement, and the closing of financially unstable family practice clinics. Fewer medical students are choosing family medicine, deterred by preceptors who are perceived to be overwhelmed and underappreciated.
What’s so bad about fee-for-service health care?
The foundation of our current care system is an outdated funding model -- fee-for-service where typically, when a family doctor provides care for a patient, they bill Alberta Health a fee for that visit, and for each time they see that patient. There is a broad consensus that this funding foundation can no longer support primary care. Because of the way the fee-for-service model works, family medicine clinics across Alberta are struggling to stay open: this model ignores rising costs and additional administrative responsibilities that are not funded. There is also broad consensus that fee-for-service funding is unable to support new and more effective models of community care.
Creating accessible and sustainable primary care.
The transformation of Alberta primary health care must begin with the transformation of our outdated funding model. Other provinces across Canada have already begun implementing alternative funding models. In February 2023, British Columbia (BC) launched its Longitudinal Family Physician (LFP) payment model: an alternative to fee-for-service where family doctors are compensated for time, patient interactions, and the number and complexity of patients in their practice.
This clinic (CVFP) provides team-based care to almost 25,000 Albertans – 30% more patients per family doctor than ‘traditional’ practices.
Here's where it gets interesting. What many Albertans don’t know is that there are alternative funding model clinics in our province and that these clinics are thriving. One example is Crowfoot Village Family Practice, located in Calgary. This clinic provides team-based care to almost 25,000 Albertans – 30% more patients per family doctor than ‘traditional’ practices. It is the most evaluated family practice in the province, showing favorable patient outcomes at a cost that saves taxpayers and the system money. An independent case study by the Health Quality Council of Alberta (HQCA), 2019, found this clinic’s funding model to be cost-effective when considering downstream healthcare system costs including emergency visits and in-patient hospital stays. Furthermore, CVFP has been growing and innovating for over 20 years, increasing the number of patients it provides care for and attracting new family doctors. The clinic model, and the resulting culture, creates opportunities to innovate. Currently, a novel strategy to provide care to some of the 4,000+ waitlist patients is being piloted.
The solution could indeed be right in front of us. Crowfoot Village Family Practice shows us that an alternative funding model with integrated team-based care is good for patients, providers, and the taxpayer. And, it shows us that the transformation of Alberta primary care should include nurturing and scaling models that are successful here and now.